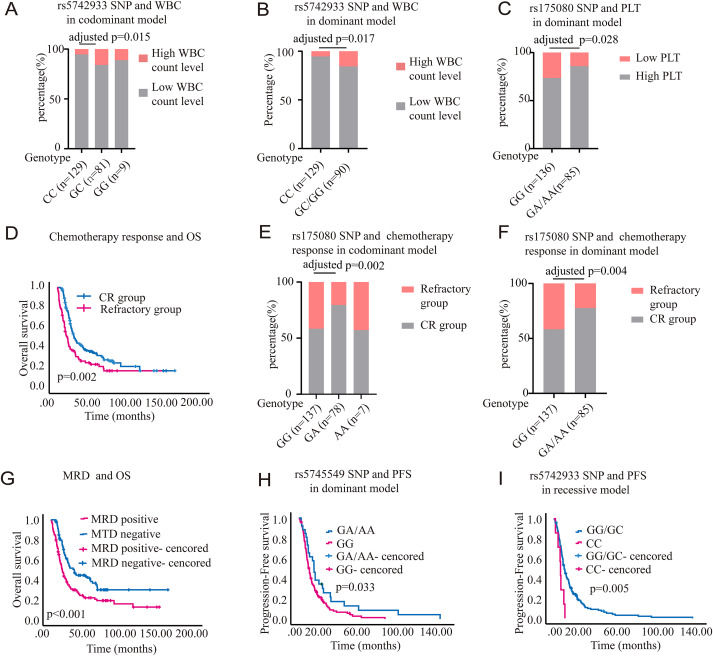
Polymorphisms of mismatch repair pathway genes predict clinical outcomes in acute myeloid leukemia patients


Acute myeloid leukemia (AML) is an aggressive hematological malignancy with a poor prognosis. Cytarabine (Ara-C), a cornerstone of AML chemotherapy, causes DNA damage.1 However, patient AML blasts can develop Ara-C resistance. Therefore, there is an urgent need to explore new targets for the treatment of AML. DNA mismatch repair (MMR) pathway genes significantly contribute to the repair process by identifying DNA damage.2 The MMR system includes several MMR proteins, such as mutL homolog 1 (MLH1), MLH3, mutS homolog 2 (MSH2), MSH3, MSH6, postmeiotic segregation increased 1 (PMS1), and PMS2. Genetic variations in MMR genes affect individuals' ability to repair chemotherapeutic agent-induced DNA damage.3 For instance, MLH1 rs1799977 AG/GG genotype displayed an increased death risk in diffuse large B-cell lymphoma.4 The GG genotype of MSH2 rs3732183 is correlated with lower recurrence risk, and the GG genotype of MLH1 rs1800734 carriers is linked with higher overall survival (OS) in oral squamous cell carcinoma.5 However, research on the prognostic relationship between MMR and AML post-chemotherapy is lacking, leading us to investigate the polymorphism of MMR pathway genes and their prognostic significance in AML.