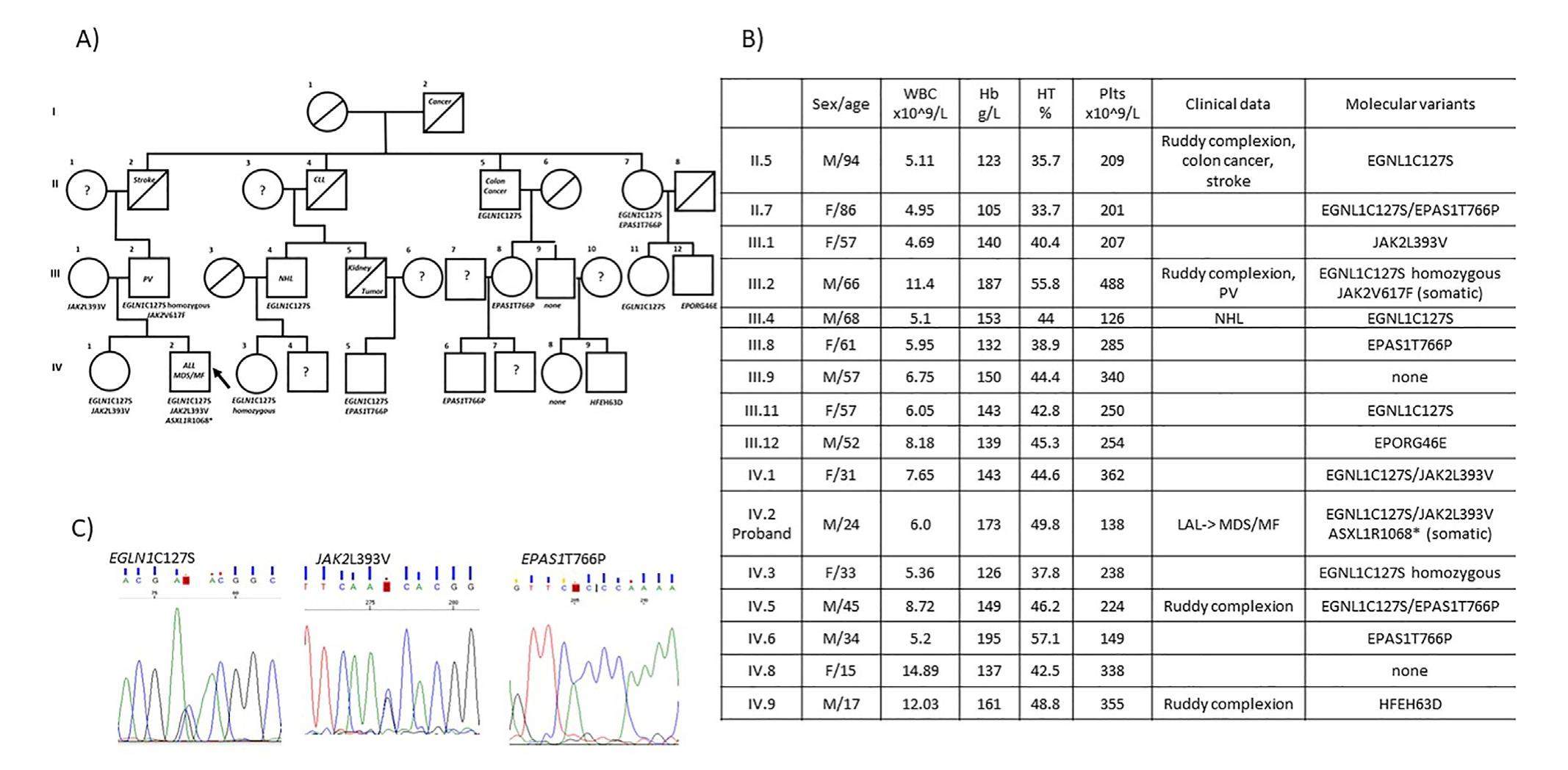
Targeted NGS analysis reveals a complex genetic background of idiopathic erythrocytosis in a large Venetian family


Absolute erythrocytosis, due to an increased production of red blood cells, becomes manifest with hemoglobin (Hb) levels above 165 or 160 g/L or with a hematocrit (HCT) above 51% and 48% in males and females, respectively. A minority of patients have polycythemia vera (PV); acquired secondary erythrocytosis frequently occurs due to appropriate or inappropriate erythropoietin (EPO) excess, while congenital secondary erythrocytosis may derive from genetic defects causing tissue hypoxia. Hereditary erythrocytosis occurs in patients with genetic mutations of the oxygen-sensing pathway (VHL, PHD2, HIF-1-alpha) or the erythropoietin receptor (EPOR) genes. Recently, HFE gene variants have been described in sporadic erythrocytoses. In a high proportion (about 70%) of patients with erythrocytosis, a specific etiology remains elusive despite extensive testing, and the diagnosis of idiopathic erythrocytosis (IE) is ruled out.